DRUGS USED TO FIGHT INFECTION
Antibacterial Drugs That Interfere With Protein Synthesis
On completion of this chapter, the student will:
LEARNING OBJECTIVE
- Discuss the uses, general drug actions, adverse reac¬tions, contraindications, precautions, and interactions of antibacterial drugs that interfere with protein synthesis.
- Discuss important preadministration and ongoing assess¬ment activities the nurse should perform on the patient taking an antibacterial drug that interferes with protein synthesis.
- List nursing diagnoses particular to a patient taking an antibacterial drug that interferes with protein synthesis.
- Discuss ways to promote an optimal response to ther¬apy, how to manage adverse reactions, and important points to keep in mind when educating patients about the use of antibacterial drugs that interfere with protein synthesis.
KEY TERMS
adjunctive treatment • therapy used in addition to the primary treatment
blood dyscrasias • abnormality of blood cell structure
bowel preparation • treatment protocol to cleanse thebowel of bacteria before surgery or other procedures; also known as bowel prep
circumoral • encircling the mouth
enteric coated • special coating on drug that preventsabsorption until drug reaches the small bowel
Helicobacter pylori • stomach bacterium that causes peptic ulcer ; also known as H. pylori
hematuria • blood in the urine
hepatic coma • coma induced by liver disease
nephrotoxicity • damage to the kidneys by a toxic substance
neuromuscular blockade • acute muscle paralysis and apnea (absence of breathing)
neurotoxicity • damage to the nervous system by a toxic substance
ototoxicity • damage to the organs of hearing by a toxic substance
phenylketonuria (PKU) • a genetic birth defect causing the amino acid phenylalanine to build up to toxic levels in the body
proteinuria • protein in the urine vancomycin resistant
Enterococcus faecium (VREF) • bacteria resistant to the drug vancomycin
PHARMACOLOGY IN PRACTICE
When taking the drug history of Mrs. Moore, an 85-year-old patient in the outpatient clinic, you note that she has been taking 0.25 mg digoxin, one baby aspirin, and the tetracycline minocycline ( Minocin ). As you read, think about possible drug interactions.
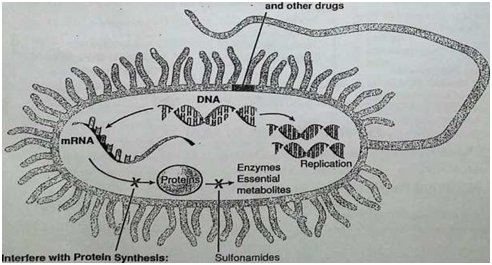
The drugs in this chapter are antibacterial agents that interfere with the development of protein (synthesis) in the bacterial cell. To make protein, a message is made by messenger RNA (mRNA) that tells the cell how to build amino acids. The message is translated by the ribosomes to make the string of amino acids that becomes a protein. These drugs act on different areas of the cell, interfering with the process of protein synthesis.
This chapter discusses - four classes of broad-spectrum antibiotics: the tetracyclines, the aminoglycosides, the mac- rolides, and the lincosamides. There are a number of newer antibacterial drugs that are a single drug in a class, and these are grouped as miscellaneous drugs. The Summary Drug Table: Antibacterial Drugs That Interfere With Protein Syn¬thesis describes the broad-spectrum antibiotics discussed in this chapter (Fig. 8.1).
TERTRACYLIN
Natural and semisynthetic compounds. They are useful in select infections when the organism shows sensitivity (see Chapter 6) to the tetracyclines, such as cholera, Rocky Mountain spotted fever, and typhus. These drags are also useful when a patient is allergic to the penicillins or cephalosporins.
Actions
The tetracyclines are bacteriostatic and exert their effect by inhibiting bacterial protein synthesis, which is a process necessary for reproduction of the microorganism. Growing resistance to the drugs is a problem with the tetracyclines
Tigecycline (iygacil) is the first drug in the glycylcycline class of tetracycline-like drugs that is more bacteria resistant.
Uses
These antibiotics are effective in the treatment of infections caused by a wide range of gram-negative and gram-positive microorganisms. Tetracyclines are used as broad-spectrum antibiotics when penicillin is contraindicated, and also to treat the following infections:
• Rickettsial diseases (Rocky Mountain spotted fever, typhus fever, and tick fevers)
• Intestinal amebiasis
• Some skin and soft tissue infections
• Uncomplicated urethral, endocervical, or rectal infections caused by Chlamydia trachomatis
• Severe acne as an adjunctive treatment
• Infection with Helicobacter pylori in combination with metronidazole and bismuth subsalicylate
Adverse Reactions
Gastrointestinal System Reactions
• Nausea or vomiting
. Diarrhea
• Epigastric distress
• Stomatitis
• Sore throat
Other Reactions
. Skin rashes
• Photosensitivity reaction (demeclocycline seems to cause the most serious photosensitivity reaction, whereas mino¬cycline is least likely to cause this type of reaction)
Contraindications:
Tetracyclines are contraindicated in the patient known to be hypersensitive to any of the tetracyclines; during pregnancy, because of the possibility of toxic effects to the developing fetus (pregnancy category D); during lactation; and in chil¬dren younger than 9 years, of age.
»' Tetracyclines are not given to children younger than 9 years of age unless their use is absolutely necessary because these drugs may cause permanent yellow-gray-brown discoloration of the teeth. The use of tetracyclines, especially prolonged or repeated therapy, may result in. overgrowth of nonsusceptible bacterial or fungal organisms.
Precautions :
Tetracyclines should be used cautiously in patients with impaired renal function (when degradation of the tetracy¬clines occurs, the agents are highly toxic to the kidneys) and those with liver impairment (doses greater than 2 g/day can be extremely damaging to the liver).