[Medical Student]: Just how inefficient is the US healthcare industry? Part 1 - Electronic Medical Records
As a medical student, I will be covering just how broken our healthcare system is as part of the “Healthcare: An Insider’s Perspective” series
If you’re from the US, you understand just how inefficient our healthcare system is: Doctors rarely show up on time; dealing with insurance companies is a headache; and keeping track of your medical record is a hassle.
Much of this defies understanding. After all, the healthcare industry is a unique outlier. While other industries - such as electronics - produce cheaper goods every year, the healthcare industry somehow manages to deliver poor quality care at ever increasing prices. Quality control in healthcare is highly questionable, and medical errors are the third leading cause of death in the US [1].
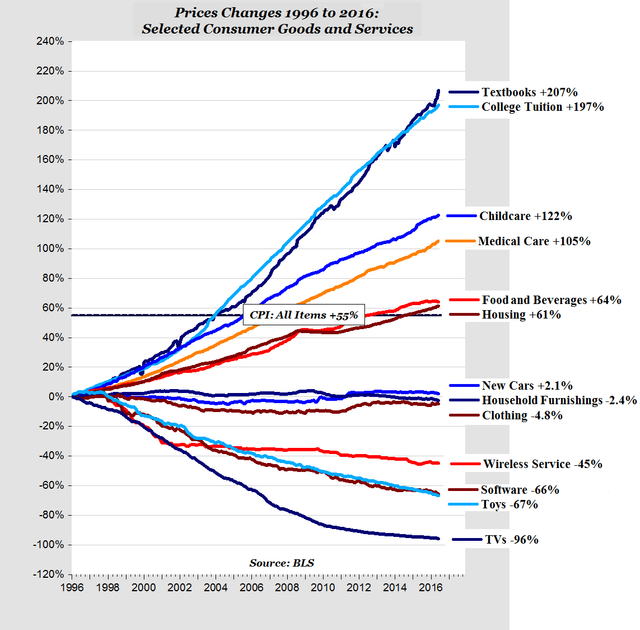
Figure 1: Medical care costs continue skyrocketing while the cost of other products, such as consumer electronics, continue to plummet. (Source: Hoosier Econ [2])
There are many reasons as to how we have arrived at this point. But here’s a significant one: Electronic Medical Records (EMRs). Absolutely reasonable in theory, but completely botched in implementation.
This is because electronic medical records were primarily designed as billing software rather than for delivering care. As a result, hospitals and doctors ignored these systems for decades in favor of paper records to track their patients - even though other industries such as finance had already adopted electronic record-keeping systems.
That changed with the passage of the HITECH Act in 2009. Devised by policymakers, who viewed the healthcare industry’s reliance on paper records as an anachronism, the act provided $27 billion dollars’ worth of subsidies (and penalties for non-adoption) for hospitals to purchase these expensive electronic medical record systems.
President Obama justified this program:
To improve the quality of our health care while lowering its cost, we will make the immediate investments necessary to ensure that, within five years, all of America's medical records are computerized...This will cut waste, eliminate red tape and reduce the need to repeat expensive medical tests.... But it just won't save billions of dollars and thousands of jobs; it will save lives by reducing the deadly but preventable medical errors that pervade our health-care system [3]

Fig 2: Obama signing the HITECH Act into law as part of the American Recovery and Reinvestment Act
Eliminating these “preventable errors” was based on the hope that these electronic medical record systems would enable physicians to instantaneously obtain patient data from other hospitals. For instance, a doctor in Oklahoma would be able to view the health records of a visiting patient from Alaska.
Ideally, this “interoperability” would allow physicians to cut down on duplicate orders for tests and prevent critical patient details from being lost in communication between different hospital systems and providers.
Reality turned out differently. While electronic medical record providers reaped the bonanza of federal dollars coming their way, they intentionally chose not to let their systems “talk” to the systems of other competing companies. Paired with the fragmented implementation of these electronic record systems due to the mandate, it wouldn’t be unusual for a hospital just down the road from another to be unable to share patient data since they were utilizing record software from competing vendors. Even today, hospitals rely on fax machines to transmit medical records to one another.
Omission of this “interoperability” was intentional: Electronic medical record companies had every incentive to do so. First, allowing their systems to be interoperable with other competitors could potentially hurt their market share. Second, the HITECH Act never explicitly required these systems to be interoperable - a critical mistake considering the bill’s multi-billion dollar price tag.
The impact on patient care - and on providers such as myself - has been immense. Relying on systems that were designed for the billing department - rather than for physicians - has hurt our ability to effectively care for our patients.
Information is fragmented and patient records at my institution are split between two separate electronic record systems. Obtaining a complete patient history - especially for elderly patients with multiple complex conditions - is a nightmare.
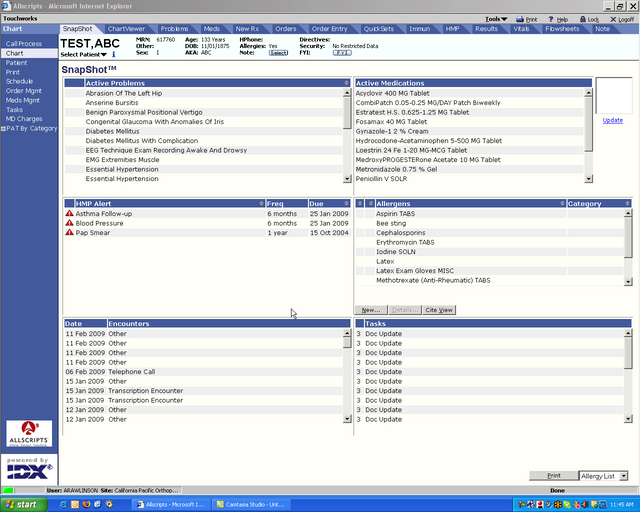
Fig 3: The interface of a leading electronic medical record. Totally not from the 1990s. Not at all
Coupled with the antiquated interfaces of these systems (which once again were never primarily designed with physicians as end users), patient care has significantly slowed down. Physicians spend more time on electronic medical record systems than they did with paper, and have less time to spare for patients as a result.
A recent 2016 study in the Annals of Internal Medicine quantified these results. Examining physician behavior across multiple specialties, it found that physicians spent only 27% of their time with patients, and a whopping 50% on electronic medical records and desk work! Additionally, these physicians were also spending an extra 1-2 hours each night on electronic medical record task-related work! [4]
This translates into greater administrative costs, decreased physician efficacy, and increased burnout. It has directly made patient care less effective and reduced our ability to care for those who need it the most.
And how are some of these systems doing nationally? Recently, the Coast Guard was so upset with its new electronic medical record system that it turned back to paper records for managing the health of its 50,000 service members! [5]
Now, don’t get me wrong: In theory, electronic medical records are a great improvement over paper records. But mandating the utilization of these systems before they were ready for clinical use - driven by questionable corporate lobbying by these electronic medical record companies for the HITECH Act - has driven up healthcare prices and lowered output per physician.
We need to drastically rethink much of our healthcare policy, and critiquing electronic medical record policy should play an important role.
If you liked this article, please upvote it!
If you have any medical topics/questions you would like me to address, please mention it in the comments below!
Sources:
[1] http://www.npr.org/sections/health-shots/2016/05/03/476636183/death-certificates-undercount-toll-of-medical-errors
[2] https://hoosierecon.files.wordpress.com/
[3] http://abcnews.go.com/Health/President44/story?id=6606536
[4] http://annals.org/aim/article/2546704/allocation-physician-time-ambulatory-practice-time-motion-study-4-specialties
[5] http://www.politico.com/story/2016/04/ehr-debacle-leads-to-paper-based-care-for-coast-guard-servicemembers-222412
@originalworks
The @OriginalWorks bot has determined this post by @benjaminrushmd to be original material and upvoted it!
To call @OriginalWorks, simply reply to any post with @originalworks or !originalworks in your message!
To enter this post into the daily RESTEEM contest, upvote this comment! The user with the most upvotes on their @OriginalWorks comment will win!
For more information, Click Here! || Click here to participate in the @OriginalWorks sponsored writing contest(125 SBD in prizes)!
Special thanks to @reggaemuffin for being a supporter! Vote him as a witness to help make Steemit a better place!