Real-life effectiveness of anti-malarial treatment regimens: what are we aiming for?
The standard of care for treating malaria is a three-day artemisinin-based combination therapy (ACT). However, specific drug resistance linked to decreased ACT efficacy has been discovered, making the clinical development of novel anti-malarial medications and medication combinations necessary.Single Encounter Radical Cure and Prophylaxis (SERCAP) had previously been suggested as the optimal target-product-profile for any new anti-malarial drug regimen because it would increase treatment adherence while also guaranteeing total cure and preventing early reinfection. This strategy might not be the best because it;
(1) requires administering an excessively large dose of the medicine to produce plasmodicidal plasma levels for a long enough period of time
(2) enhances the possibility of harmful medication responses, and
(3) gives the patient a single chance to receive a cure—or not—by taking a single dose of medication. Promising drug research programmes have been put on hold as a result of SERCAP in recent years, and needless attrition in the pipeline for developing anti-malarial drugs has resulted.
One argument would be the idea of single-day multi-dose regimens as a possibly superior substitute because they;
(1) use a lower dose of the medication at each time-point for improved safety and tolerability,
(2) improve treatment compliance based on taking the anti-malarial medication within 24 hours while the symptoms of malaria are still present, and
(3) have more than one opportunity for adequate intake of the drug in case of early vomiting or other factors causing reduced bioavailability.

According to a recently published critical stance on the idea of SERCAP, an alternate suggestion is to aim for multiple-dose anti-malarial therapy regimens lasting less than three days in place of the present World Health Organisation (WHO) treatment recommendations. This may make it easier to achieve the best possible balance between enhancing treatment adherence, maximising therapeutic effectiveness, and minimising the attrition of new medications and medication regimens.
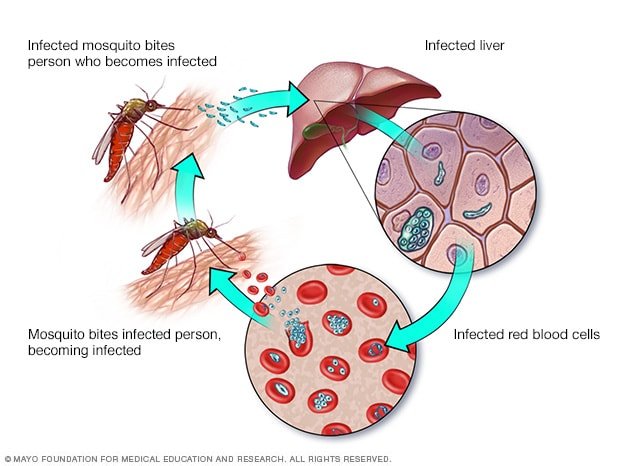
The recommended malaria treatment for the past 20 years has been an artemisinin-based combination therapy (ACT), administered for three days. ACT is less effective in clinical settings than it is in research settings, though. This is caused by a number of things, like improper administration or disregard for the recommended course of treatment.
Even when information and resources are accessible, a rapid therapeutic response or the incidence of adverse medication responses associated with treatment may cause a patient to stop taking the prescribed treatment regimens too soon. While ACT is still quite effective in sub-Saharan Africa, there have been reports of clinically significant delays in parasitological response and the establishment of molecular resistance indicators.
Thus, there is a critical need for innovative, efficient therapies that are secure, well-tolerated, and characterised by straightforward, condensed regimens.
Based on this knowledge, the idea of single-dose treatment for uncomplicated malaria was developed, and this idea served as the foundation for the clinical drug development of novel anti-malarial drug candidates .The agreed-upon target product profile in the development of anti-malarial drugs for the past ten years has been single-exposure radical cure and prophylaxis (SERCAP). One of the largest international collaborative efforts for the development of anti-malarial drugs, the PAMAfrica consortium, for example, plans to create a single-dose multi-drug combination using the largest anti-malarial drug portfolio ever, which will be managed by the Medicines for Malaria Venture (MMV). Similar to this, the SINDOFO consortium has an explicit goal of creating a single-dose therapy using a pharmacological class other than ACTs.
By administering just one dose of the anti-malarial, SERCAP aims to solve the issue of inadequate treatment adherence.
In a recent opinion piece, Professor White makes the argument that the requirements for new drug candidates to meet SERCAP criteria are overly stringent, which may actually work against the development of novel anti-malarial medicines. A single-dose cure poses a pharmacological challenge in and of itself because the administered dose must be excessively high to produce therapeutic plasma drug concentrations over a long enough period of time, account for inter-individual variations in bioavailability, and ensure that patients without significant semi-immunity, such as children, are cleared of parasites without posing any pertinent safety issues.

The chance of experiencing a typical three-day treatment course's unpleasant drug effects, such as early vomiting, is inevitably increased by doing so. As a result, the patient may not have enough blood concentrations to effectively eliminate infection. The idea of SERCAP may have been the primary factor in the early attrition of the clinical drug development of promising new anti-malarial drug candidates, such as arterolane or artefenomel, or drug combinations including artefenomel-piperaquine and artefenomel-ferroquine. This is true even though overall it ensured increasing quality of new drug candidates.
The desire for a single-dose treatment may therefore postpone or even prevent the development of new anti-malarial drugs. Therefore, Professor White urges keeping three-day treatments as the primary objective for new anti-malarial medication regimens similar to the first-line ACT.

While the systematic assessment of three-day, two-day, and one-day regimens is welcome, SERCAP should not constitute the ultimate goal of anti-malarial drug development. Instead, funders should also encourage development of multiple-dose regimens that are ideally administered within a single day. Developing drug candidates as a multiple-dose single-day anti-malarial combination therapy will reduce attrition of new drugs while maximizing the potential benefits in effectiveness of new drug regimens.
Abbreviations
ACT:
Artemisinin-based combination therapy
AUC:
Area under the curve
G6PD:
Glucose-6-phosphate-dehydrogenase
MMV:
Medicines for malaria venture
SERCAP:
Single-exposure radical cure and prophylaxis
TPP:
Target product profile
Thank you for reading and hope you got some value
Kndly SUBSCRIBE to our YouTube channel for more contents.
https://youtube.com/@TheMindsetShift8