Differentiating Nephrotic Syndrome and Nephritic Syndrome
This was a topic i used to find quite challenging when I started studying nephrology. So in this post i'll try to simplify it as much as I can.
Both nephrotic and nephritic syndromes involves pathology of the glomerulus. That is, somehow, the glomerulus is damaged, which results in either of these syndromes, depending on the specific type and mechanism by which the damage occurs.
First let's look back at the basic structure of the glomerulus.
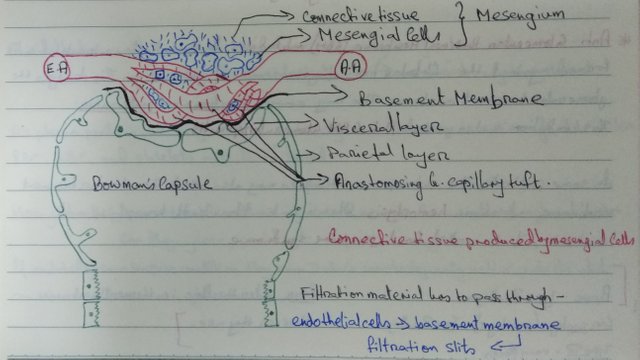
The visceral layer of epithelial cells have special features called podocytes. Podocytes are finger like processes that project out from these cells and create a slit like openings surrounding the glomerular capillaries. Let's look at a slightly more detailed image (from Goljan Rapid Review Pathology, 4th edition)
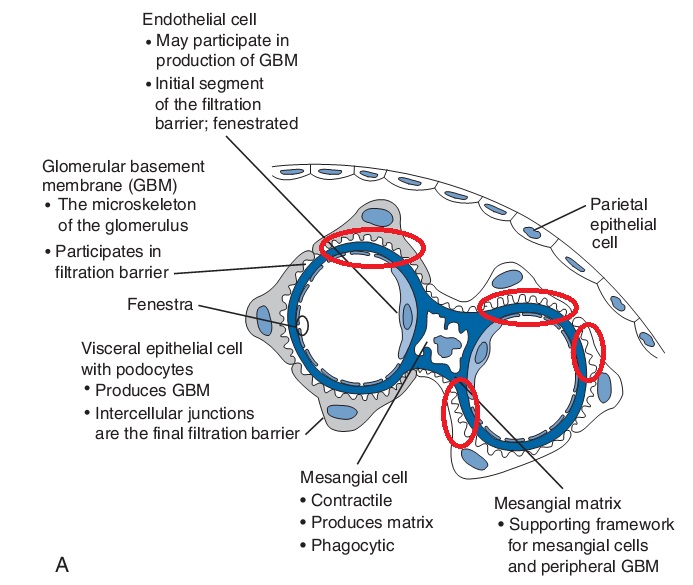
The red circles are the slit like openings. These slits are very narrow and forms part of a filtration barrier. This filtration barrier is the reason why not a lot of proteins can filter through the glomerulus into the tubules. This filtration barrier ensures only very small particles are allowed to pass through into the glomerular filtrate and into the PCT. (You already know this bit if you have read the previous post on how urine is produced)
Also, not a lot of cells from the blood in the capillaries, like the red blood cells (RBCs) and white blood cells (WBCs) can filter through as well. This is ensured by the presence of only very tiny fenestrations between the endothelial cells of the glomerular capillaries. (Note that these are NOT the epithelial cells). Let's look at another image from my notes!!
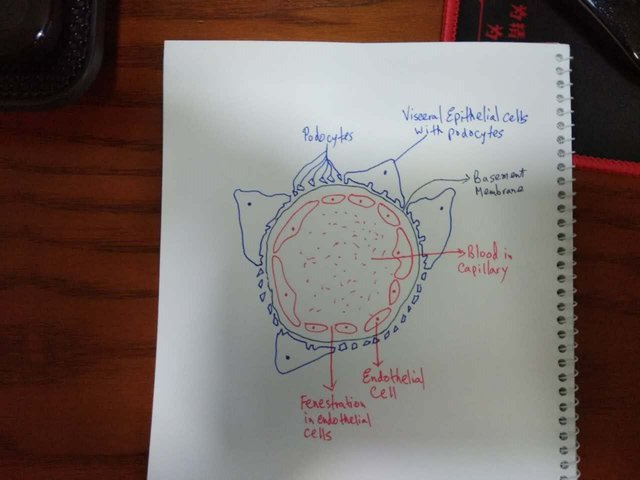
The endothelial cells provide the initial barrier to large cells like RBCs and WBCs. The epithelial cells with podocytes provide the major barrier to large proteins like albumin. These two provide a size barrier, i.e. these filter substances according to size. In the image above, you will also see a basement membrane which is negatively charged. The basement membrane provides a charge barrier, in the sense that any substances which is negatively charged will not be able to pass through it. As it happens to be, most plasma proteins are negatively charged!! Together these 3 components form the filtration barrier and ensures most cells and proteins in the blood are not filtered.
NEPHROTIC SYNDROME :
Now imagine what might happen if something damages the podocytes. The filtration barrier will no longer be as effective and large proteins, mainly albumin, which were not able to filter through with an intact filtration barrier, will now start filtering through and appear in the urine (Note that most likely these substances will not be reabsorbed back in the nephron, because, as these substances are not supposed to filter through, our nephrons are not equipped to reabsorb most of these substances).
This is exactly what happens in nephrotic syndrome. Via some disease process, the podocytes are either damaged or lost or are not working properly anymore. Bottom line, the function of the podocytes are lost somehow.
As a result, they are not able to keep the protein in. As a result, there is a loss of large amounts of protein in the urine (>3.5g/Day). This massive proteinuria has it's consequences. The symptoms of nephrotic syndrome arise mostly as a consequence of this massive loss of protein.
One of the first symptom that appears is frothy urine. Now, don't get alarmed if your urine is slightly frothy, because a small amount of protein in the urine (<150 mg/day) is considered normal. But if it's significantly frothy, you might wanna consult your physician.

image from google
Because a lot of protein is lost in the urine from the blood, the colloid osmotic pressure inside the blood vessels all over the body decreases and the hydrostatic pressure is now relatively higher. This results in a net force which is directed outwards from the blood vessels and fluid from the vessels will be forced out into the interstitial spaces all over the body. Thus these patients will have edema all over the body, which significantly manifested as puffy eyes and swelling of the lower limbs.
Albumin is one of the major proteins that is being lost, and when albumin is lost, the liver compensates by overproducing lipids. So the patients will also have hypercholesterolemia and hyperlipidemia. (The mechanism of this is still not quite clear).
As there is increased in lipids in the blood, we might see fatty casts or oval fat bodies on urine examination.
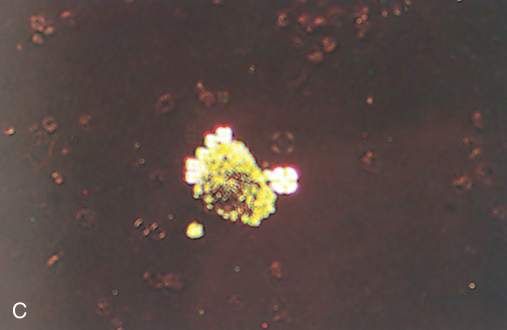
image from goljan rapid review pathology
Another very important protein that is being lost is Antithrombin III (AT III). AT III is a major anticoagulant. Loss of AT III leaves the patient in a very hyper coagulable state. Thus the patients will be at increased risk for conditions like renal vein thrombosis, deep vein thrombosis and pulmonary embolism.
Nephrotic syndrome may arise from primary glomerular diseases or secondary causes.
Primary Glomerular diseases :
Membranous Glomerulopathy
Minimal Change Disease
Focal Segmental Glomeruloslerosis
Diffuse Proliferative Glomerulonephritis (DPGN)
Membranoproliferative Glomerulonephritis (MPGN)
Secondary Causes :
Systemic Diseases such as Diabetes, Amyloidosis and SLE
Drugs such as NSAIDs, penicillamine and heroine
Infections such as malaria, syphillis,_ Hepatitis B and C and HIV
Malignancies such as carcinoma, lymphoma
Allergy, Hereditary nephritis
NEPHRITIC SYNDROME
Now let's imagine what might happen if the endothelial cells are damaged. The endothelial cells provided the primary barrier to RBCs and WBCs. Thus if the endothelial cells are damaged, these cells will start appearing in the urine.
Nephritic syndrome is basically the result of an inflammatory response to immune complexes that lodge themselves at the glomerular capillaries. The body directs an immune response by recruiting WBCs, mainly neutrophils, againsts these immune complexes in the glomerular capillaries. As a result there is inflammation in the glomerular capillaries which damages the endothelial cells.
As the endothelial cells get damaged, at some places large openings are created between cells which allow RBCs and WBCs to filter through and into the nephron and eventually appear in the urine. This is manifested as hematuria (blood in urine) and pyuria (white blood cells in urine). On urine examinations we might also see casts of RBCs and WBCs.
RBC cast
.jpg)
image from goljan rapid review pathology
WBC cast
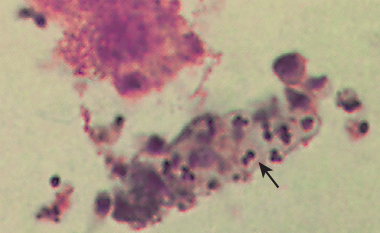
image from goljan rapid review pathology
If these newly created holes are large enough for cells to go through, then these are also large enough for some proteins to go through as well. Thus we will also see some proteinuria, although it will be less than what we'll see in nephrotic syndrome (>150mg/day, but <3.5 g/day) because the podocytes are still functioning properly in nephritic syndrome. So in nephritic syndrome, we might see the signs and symptoms we saw in nephrotic syndrome, but to a much lesser extent. (But, If the disease gets too severe and podocytes starts losing their function as well, then we might see nephrotic range of proteinuria and the symptoms associated with proteinuria will be as severe as in nephrotic syndrome).
As the disease progresses and the glomeruli are getting inflammed, it's going to affect the free filtration of fluid into the nephron. The inflammed glomeruli are not very effective at filtering the normal substances and the glomerular filtration rate (GFR) decreases. Thus there will be decreased urine production, known as oliguria. Thus there will be retention of fluid and salt (NaCl) in the vessels. Retention of fluid and salt will eventually lead to hypertension.
Retention of fluid will also increase the hydrostatic pressure inside the blood vessels and as a result, we will see edema in nephritic syndrome as well. (But note that the mechanism of the edema in nephritic syndrome is entirely different that the mechanism of the edema that happens in nephrotic syndrome).
Similar to nephrotic syndrome, nephritic syndrome may also arise from primary glomerular diseases or secondary causes.
Primary Glomerular Causes :
Rapidly Progressive Glomerulonephritis
Berger's Disease
Diffuse Proliferative Glomerulonephritis (DPGN)
Membranoproliferative Glomerulonephritis (MPGN)
Secondary Causes :
Acute Post-Streptococcal Glomerulonephritis
_Alport Syndrome, SLE
Note that DPGN and MPGN can present as either nephrotic or nephritic syndrome.
To simplify this long complicated topic :
- If we see massive proteinuria with no associated cells or casts in the urine, think nephr"O"tic syndrome. If there's presence of RBCs, WBCs, casts or inflammatory cells in the urine, think nephr"I"tic syndrome.
- Because Acute Post-Streptococcal Glomerulonephritis is a common cause of nephritic syndrome, there is usually a history of recent throat infection (pharyngitis) or skin infection associated with nephritic syndrome. This is not present with nephrotic syndrome.
- Hypertension is usually seen in nephritic syndrome. It is usually absent in nephrotic syndrome.
- Hematuria is present in nephritic syndrome, not nephrotic syndrome.
Sources :
Goljan Rapid Review Pathology, 4th Edition
Robbins Basic Pathology. 8th Edition
First Aid for USMLE Step 1
Alright guys, that's it for now!! Hope you learned something today!!
Start Upvoting to increase your Curation Rewards. Resteem this post and maybe more people out there might find this useful.
If you enjoy medical topics, health tips, or steemit tutorials for beginners and newbies, please make sure to follow me at @simplifylife
Peace!!
Can a Physicisn damage the glomerulus while performing an operation? A few years back i was diagnosed with cushings syndrome. The tumor was in my right adrenal gland. They removed the whole adrenal gland. I was cured of the cushing syndrome but sometimes now my urine is quite frothy and especially in summer i get water retention in my feet. Do you think it would be wise for me to go back to my endochronologist?
the kindeys are covered by capsule and perinephric fat. Glomerulus are deep inside to these structures. Performed correctly,shouldnt be a problem. Fact: A human can still function normally without one kidney and the other working at 1/3rd its capacity.
There is always a risk of slight injury, but not to a very severe extent. But if you're having significant frothy urine and water retention regularly, you should see a nephrologist. And yes, you should also see your endocrinologist for a follow up visit.
I wish you stay healthy and strong :)
i student in my school days in biology class about neprotronic syndrome :)
I hope this post helps you nail this topic in your biology class xD xD
Your write up is impressive. Followed @simplifylife
Thank you very much!! I'm glad you enjoyed the post :)
Resteemed.
Thank you so much!! Really appreciate the support!!
Join us on #steemSTEM / Follow our curation trail on Streemian
Thank you for this very interesting article that we took a great pleasure to upvote. Please visit our chat channel for more interactions with us!
The steemSTEM project is a community-supported project aiming to increase the quality and the visibility of STEM (STEM is the acronym for Science, Technology, Engineering and Mathematics) articles on Steemit.
Thank you so much!! Just joined the steemit chat channel :) Hope to connect with more authors there :)
I see you're doing great work! :D
Well done!
Hehe i've kept your suggestions in mind :) :)
Keep it up my friend! Keep it up! ;)
Will do my best :) Thank you so much!!
nice post,awesome write up.followed
Thank you very much :)
I studied the urinary system on my physiology class last university year. Now reading your post I finally understood whats all about nephritic and nephrotic syndromes, always got confused when I saw them on the pathology annotations. Thanks! Looking forward for further posts.
I'm glad this was helpful :) Thank you very much.
Thank you for this post!
You're welcome!! I hope you found this post helpful :)
Informative and interesting..