Brachytherapy in the treatment of cervical cancer.
Brachytherapy plays an essential role in the treatment of invasive cancer in the cervix. In radical treatments, it is usually combined with external beam treatment, but it can also be combined with preoperative or postoperative surgery. More recently, internal radiotherapy has been combined with simultaneous platinum-based chemotherapy in cervical cancer [1]. It is mainly applied as an intracavitary procedure, in selected cases supplemented by interstitial implants. Radical brachytherapy for cervical cancer is always based on the use of intrauterine and intravaginal sources.
For patients to receive internal radiation in that area, an instrument called applicators is used, which allows the insertion of the radioactive source or seeds, which are generally used iridium-192 and cesium-137.
In the case of applicators we have 3 types which are [2]:
Manchester:
The classic technique of Manchester was based on the use of an intrauterine tube with the option of two standard lengths (4 cm and 6 cm) and a non-standard length (3.5 cm) (each tube has a rubber flange at its cervical end). to keep the tube in the correct position) and two ellipsoid vaginal ovoids in shape, two small (2 cm), two medium (2.5 cm) or large (3 cm) in diameter kept separated in the vagina by a washer or a spacer. Modern Manchester applicators physically imitate the classical technique.
The intrauterine tubes have the same fixed lengths and fixed cervical flanges and have an angle of 40 degrees with respect to the line of the vaginal component of the tube. The vaginal ovoids have retained their ellipsoid shape (large, medium, small, medium) with small ovoids subsequently extended by 5 mm to form a filling inside them. These three afterload tubes are held together and their relative positions are fixed by a clamp that ensures an ideal physical arrangement.
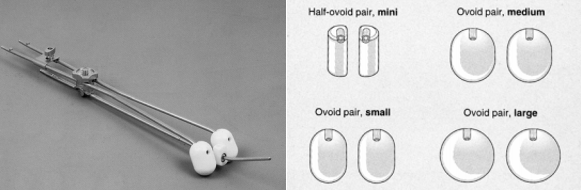
Figure 1. Manchester applicator and ovoid set [2].
Fletcher:
In the early 1950s, Fletcher developed a radio system that combined a rigid metal intrauterine tandem with cylindrical colpostats; The latter are positioned against the cervix, perpendicular to the axis of the vagina. Subsequently, this system was modified by Delclos and Game for manual loading and then for remote post loading (Fletcher-Suit-Delclos applicator).
Later, Horiot proposed a European version to adapt it to the use of cesium sources and different afterload machines. The intrauterine tandem is available in a variety of curvatures. The length can be adjusted by positioning an adjustable flange. The cylindrical colpostats are 2 cm in diameter, but can be enlarged by adding caps of 2.5 or 3.0 cm in diameter. The tungsten shield is integrated in the front and back of the standard colpostats to reduce the dose to the bladder and rectum. Tandem and colpostats are selected to fit the volume of the tumor and the topography and individual anatomy of the patient. The position of the applicator is maintained by a vaginal packing that is also used to reduce the dose to the bladder and rectum.
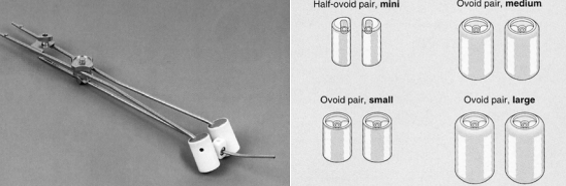
Figure 2. Fletcher applicator and ovoid set [2].
Stockholm:
The classic "Stockholm method" was based on a flexible intrauterine tube and a flat box (plate) in the vagina pushed by an individual packing device against the cervix. The tube and the box were implanted independently of each other. Therefore, there was no fixed geometry present. The rigid uterine tandem with a ring applicator was developed during the 1960s as a posterior charge device, first for sources of cesium-137, and then also for iridium-192.
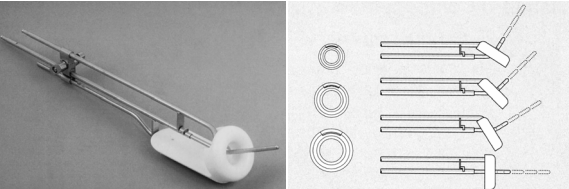
Figure 3. Classical metal ring applicator set and lengths and angles of the intrauterine tube [2].
Advantages of brachytherapy applied to gynecological cancer; radiation administration:
Standard of medical attention: it is considered a standard of treatment in gynecological cancers.
Accuracy: personalized radiation administered precisely to the target tumor.
Proven efficacy: cancer control and survival rates equivalent to EBRT (external radiation therapy) and surgery at certain stages of the tumor.
Minimization of side effects: avoid unnecessary radiation in healthy surrounding tissue to minimize side effects in the intestine and bladder and obtain favorable functional results.
Advantages for quality of life: Much shorter duration of treatment and improvement in quality of life compared to the EBRT.
Advanced techniques: Brachytherapy is continuously improving thanks to advances in imaging techniques, computerized planning technology and the design of the applicator, which increases accuracy and efficiency and reduces mortality.
Profitable: favorable profile in terms of investment, maintenance and profitability.
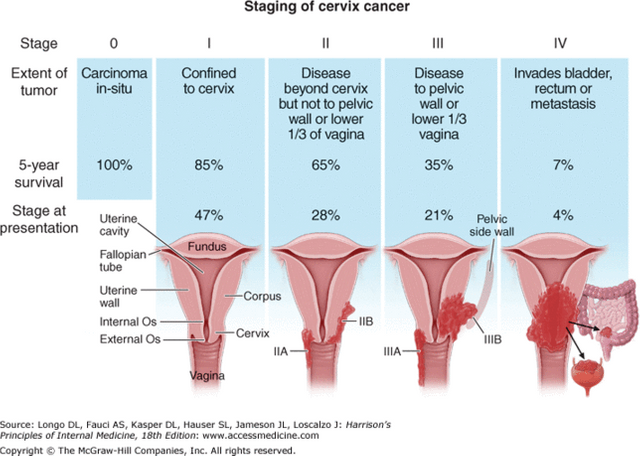
Figure 4. Types of precancerous stage and the subdivision of these [3].
Complications of Brachytherapy that can be presented to a patient.
Acute: present in the first week or two after implant and is due to damage to the cells of the organs at risk, resulting in cystitis, diarrhea, rectitis, vaginitis and dermatitis in external genitalia.
Chronicles: presented one month after the application of the last implant and is due to the repair of the cells of the organs at risk, resulting in vaginal synechiae, chronic rectitis, chronic cystitis and vaginal dryness.

Figure 5. Insertion of the applicator in a patient [2].
REFERENCE.
[1] Green JA, Kirwan JM, Tierney JF, et al. Survival and recurrence after concomitant chemotherapy and radiotherapy for cancer of the uterine cervix: a systematic review and meta-analysis. Lancet 2001; 358: 781-6.
[2] Gerbaulet. A, Pötter. R. (2002). The GEC ESTRO Handbook of Brachytherapy. ISBN 90-804532-6
[3] Cervical cancer at cancercervical.wikispaces.com.