Necrotizing Fasciitis; The flesh eating disease- it’s brief history, causes,diagnoses, prevention, treatment,mode of entry etc. Warning:The images shown here are sensitive and gross
INTRODUCTION
I was surfing the internet when I saw a picture of a man diagnosed with this life threatening infection -(necrotizing fasciitis) and decided to research on it and share it here. I want to create awareness because I’m positive most of us do not know that a flesh eating bacteria is in existence.
You could be thinking, Do the bacteria literally chew flesh? Of course not. They typically release toxins which makes the soft subcutaneous tissue die.
The Necrotizing Fasciitis also called the flesh eating disease is an infection that can lead to the death of the soft tissue(Necrosis). It is an inflammatory disease that spreads rapidly, the necrosis moves along a facial plane and it’s rapid increase is relative or proportional to the thickness of the subcutaneous tissue (the tissue beneath your skin).It is a very severe disease that occurs abruptly.
Brief history
The first case of the flesh eating disease was noted in the 5th century BC, the Hippocrates described the disease as a critical infection which generated swellings,disgusting discoloration and slough of a person’s face which was later identified as Necrotizing erysipelas.
Necrotizing fasciitis is a very rare disease but could be easily contacted by one. It is highly fatal unless diagnosed on time and treated properly.
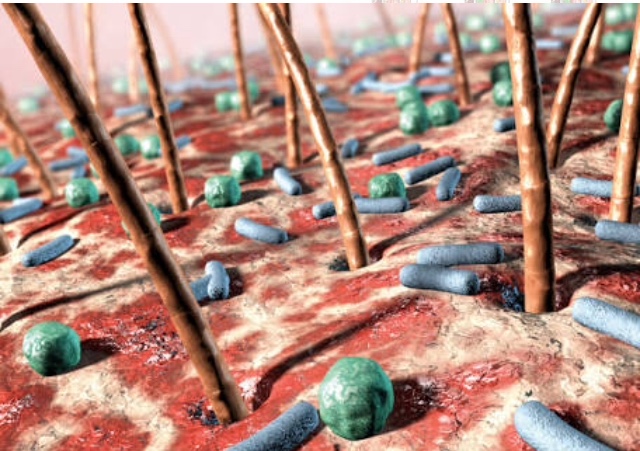
MODE OF ENTRY OF THE BACTERIA
An open wound is the main point of entry of this flesh eating bacteria. When it enters the body, it doesn’t literally chew the flesh of the host as the name may imply but rather releases toxins to aid in the death of the subcutaneous tissues of the host. Once the tissue is dead, it goes into the bloodstream which aids in its movement and rapid spread.
Bacteria responsible for Necrotizing Fasciitis
These bacteria are the relative cause of Necrotizing Fasciitis and they include group A Streptococcus (group A strep), Klebsiella, Clostridium, Escherichia coli, Staphylococcus aureus, and Aeromonas
hydrophilla. The sever form is caused by
Streptococcus pyogenes.


Is Necrotizing fasciitis communicable or contagious?
Necrotizing fasciitis is only gotten when there’s an open wound or cut, just the way regular infections are gotten.
It is not exactly communicable nor contagious, nonetheless it could be transmitted from human to human through the exchange of respiratory secretions or by entering an open wound.
INFECTIVE PROCESS
Scientists classify necrotizing fasciitis into types which includes;
The ‘types’ are the infective process of the necrotizing fasciitis disease and are divided into four types; TYPE I, TYPE II, TYPE III and other organism. The TYPE II is the most sensational.
Type I : Here the Necrotizing Fasciitis occurs as a secondary entity to an existing infection as it is usually related with sub-acute infection. There is usually a presence of at least one anaerobic species of the bacteria which include Bacteroides, Clostridium or Peptococcus. Either of these anaerobic bacteria could be present in isolation in combination with one or more aerobes which could be either Escherichia coli, non-Group A Streptococci, Klebsiella or Proteus.
In this ‘Type’ the host’s immune defence is defeated as the anaerobes bacteria and aerobes bacteria work in synergy to fulfil that purpose.
Type II: Necrotizing fasciitis is the most common type as it has been the one of most interest in the media and is commonly referred to as flesh-eating disease. All age groups and healthy people are prone to this life threatening disease.
This disease is normally suspected when acute and fulminating
infection is identified. Cases like this often arise from an unknown source and the point of entry of the organisms may not be clearly revealed or known.
Group A Streptococci, either in isolation or in combination with Staphylococcus aureus, are a mostly found to be the bacteria causing this disease in Type II.
TYPE III : The bacteria Clostridia perfringens or Clostridia septicum is the causative bacteria in this ‘type’ of necrotizing fasciitis. It enters the body through injury or surgery which leads to formation of gas under the skin, in this process produces a sound called crepitus. People who inject “black tar” heroin subcutaneously are prone to clostridia infection and the development of the flesh eating disease.
Other organisms :
Necrotizing fasciitis can be contacted due to other organisms , specifically marine organisms. The disease gets inside the person’s body through the contamination of the wound or cuts on the person’s body by sea shells and other sharp Sea object. Patients with liver disorders are at a higher risk of contacting this infection and if not diagnosed promptly and treated properly, it can be very critical.
Other terms used for necrotising fasciitis include ;
- Meleney ulcer,
- haemolytic streptococcal gangrene,
- acute dermal gangrene,
- Suppurative Fasciitis
- hospital gangrene,
- and synergistic necrotising cellulitis
SYMPTOMS OF NECROTIZING FASCIITIS
Other terms used for necrotising fasciitis include ;
- Meleney ulcer,
- haemolytic streptococcal gangrene,
- acute dermal gangrene,
- Suppurative Fasciitis
- hospital gangrene,
- and synergistic necrotising cellulitis.
The initial symptoms of necrotizing fasciitis
Skin may become warm or red and patient may feel muscle pull
Patient may feel like they have a flu
Patient may develop a painful, red
bump(it grows quickly if not treated
promptly), which is mostly small in size.
Discoloration of the skin as it decays and oozing of the affected area.
Skin lesions may appear.
fatigue
weakness
fever with chills and sweating
nausea
vomiting
dizziness
infrequent urination
Critical symptoms of necrotizing fasciitis



IMAGE F showing a woman diabetic woman infected with necrotizing fasciitis
30% of the people infected with this disease develop hemorrhagic bullae which may cause them to become anemic.
The critical symptoms are seen in the last stages of Necrotizing Fasciitis.
There is a fatal decrease in the patient blood pressure as the body becomes too weak to fight off the infection, unconsciousness sets in, in the process.
There is progressing gangrene in the infected area. Due to the action of the bacteria in the damaging of the patient nerve, the patient may become numb.
Heart failure, renal failure and respiratory failure may occur due to the toxins released into the body by the bacteria.
Inflammation of the skin is noticed in affected area resulting in necrotic eschars that look like deep thermal burn.
DIAGNOSIS AND TREATMENT OF NECROTIZING FASCIITIS
Diagnosis:
• Prompt diagnosis is somewhat difficult as the disease often looks like a boil or simple skin infection in its initial stage. Laboratory and Imaging modalities could raise the belief that necrotizing fasciitis is present in the patient. When you’re not sure of the patient’s status, a small "keyhole" incision can be made into the affected tissue, and if a finger easily separates the tissue along the fascial plane, the diagnosis is confirmed and an extensive the removal of the dead tissue should be performed.
- The use of antibiotics to kill the bacteria.
- Debribement of the affected area
- use of surgical method by amputation.


IMAGE F showing the before and after treatment of the type II NECROTIZING FASCIITIS
Prevention
Proper wound care and good personal hygiene.
Risk factors
Patient’s which one of these factors stated below are the most prone or susceptible to the infection.
- Poor immune function such as from
- diabetes or cancer,
- obesity,
- alcoholism,
- intravenous drug use, and
- peripheral vascular disease
Conclusion
The Necrotizing Fasciitis also known as the flesh eating disease is a life threatening skin infection that should be prevented. The mortality rate of ‘type II’
is high and affects all ages and also healthy people but those with immunodeficiencies are more prone to it.
It’s a threat to humanity and should be prevented and if contacted diagnosed promptly and treated aggressively.
THANKS FOR READING!
References
Necrotizing Fasciitis
Brief history
Bacteria responsible for Necrotizing Fasciitis
Is Necrotizing fasciitis communicable or contagious?
SYMPTOMS OF NECROTIZING FASCIITIS
Critical symptoms of necrotizing fasciitis
DIAGNOSIS AND TREATMENT OF NECROTIZING FASCIITIS
Image sources
IMAGE F showing the before and after treatment of the type II NECROTIZING FASCIITIS





Nice post dear. Thanks for sharing this
Goosebumps all over me 😨😨. Wow!
@florae whats your inspiration behind this post. Like seriously, disease plenty oh... This is my first time I am hearing of this kind of disease. At least, you have outlined the measures to adhered to in order to prevent the prevent.
Meanwhile, this is highly educative and informative
Ouch, my stomach curled up after I saw this..... Quality post, just couldn't read all of it...
I’m sorry about your stomach lol
eeew. Very informative post. Thanks for sharing
Thank you
Please add a warning to viewers as some of the pictures are of a graphic nature.
Thank you
I just did .
It would be nice in the title. Thank you.
Done @greenrun. Thank you for the heads up
Thanks a lot.
Honestly, I have never seen things like this. You have done a great job, keep it up.
This is a test comment, notify @kryzsec on discord if there are any errors please.
Being A SteemStem Member